Top surgery included in leading breast surgery textbook for first time ever
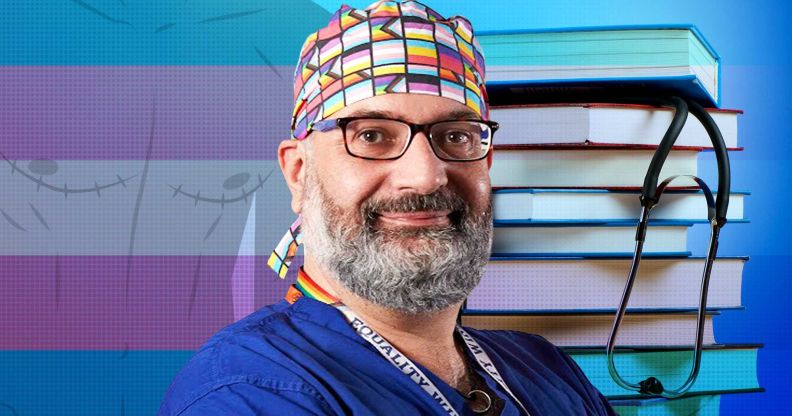
Ioannis Ntanos, one of the UK’s top gender affirmation surgeons, says the inclusion of a section on top surgery fills a ‘massive’ gap in trans healthcare education. (Getty/Nick Freeman, 246 Photography)
Top surgery is being included in a leading breast surgery textbook for the first time ever – and for Ioannis Ntanos, one of the UK’s leading gender affirmation surgeons, this moment plugs a “massive hole” in education for healthcare professionals to properly care for the trans population.
Breast Surgery, which is part of the Companion to Specialist Surgical Practice series, is an up-to-date and practical reference guide providing the latest updates on surgical practice for those going through surgical training to established consultants.
Now, the seventh edition of the vital reference includes information about top surgery, a procedure that augments or removes breast tissue to create a more masculine-contoured chest for trans men and non-binary people.
Ntanos, who contributed the top surgery section to the textbook, tells PinkNews that he bought an earlier edition of this book as a reference for breast surgery when he started his general surgical residency in 2005.
Back then, there was no mention of top surgery or gender-affirming healthcare for trans people. So he says having a resource on gender-affirming care in a major surgical textbook is much more than just a “tick box” exercise for medial professionals.
“There is no structured curriculum in the undergraduate education, no structured curriculum in the postgraduate or specialist training,” Ntanos says.
“Unless you are extremely interested on your own or by luck, you end up in a unit with someone who has been performing gender-affirming care for some time, you might spend all your years in training and never encounter the fact that there is this type of care as well.
“There is training in inclusivity in LGBTQI+ issues. Sometimes this is just a tick box.
“Sometimes it’s just a token, ‘Yeah, we’ll have that on the curriculum too.’ Sometimes it’s not designed as it should be.”

Medical training on trans healthcare, including top surgery, is sorely lacking
Only 41 per cent of medical students reported having any teaching on LGBTQ+ healthcare, according to a 2023 study of 28 UK institutions. A majority (97 per cent) said this was a one-off or irregular session.
A 2011 survey of over 170 US and Canadian medical schools found their students received a median of just five hours of LGBTQ-related training.
In 2014, the Association of American Colleges said US and Canadian medical schools need to provide better training on LGBTQ+ healthcare.
For Ntanos, it’s crucial that gender-affirming care, including top surgery, is included in the medical school curriculum because it not only helps trans, non-binary and gender diverse patients – it also helps clinicians to “become better professionals”.
“What we offer in gender-affirming care – this personalised care, this life-changing care – will make us better when we can see the result of it, to appreciate the care we offer,” the surgeon says.
“In a romantic setting, we all went into medicine to help others.
“In my experience, since I got involved in gender-affirming care in 2017, that feeling of helping others is back.
“Some volume of it was lost during the years because of rotas, weekends, long shifts and whatever. It came back because of the feedback of the patients that we offer our care.”

Ntanos says gender-affirming surgeries are an example of how patient-centred care is not only crucial for trans people but for anyone undergoing surgery.
He describes top surgery and gender-affirming care as involving work which goes “beyond the everyday” of what breast surgeons and plastic surgeons do for patients, who could be going through cancer treatment.
Working with trans, non-binary and gender diverse people involves having to be “familiar with who that patient is” and knowing that “one size does not fit all” when it comes to surgical outcomes.
That hyper-focus should be an example of how “personable” care should be for every patient, Ntanos says.
Still, medical care for the LGBTQ+ community, particularly trans individuals, has become heavily politicised worldwide.
MPs in the UK have attacked gender-affirming healthcare for trans youth while the Conservative Party repeatedly uses the trans community as a political football.
Several Republican presidential candidates – including Mike Pence, Donald Trump and Vivek Ramaswamy – promised to launch restrictions on trans healthcare if elected to the Oval Office in 2024.
Trans people struggling to get the care they need
Trans, non-binary and gender non-conforming people find themselves on years-long waiting lists, have to endure invasive questioning at clinics and confront additional barriers to other aspects of healthcare because of their identity.
Ntanos feels the discussion about trans healthcare has “gone off the rail for too long”. There’s ample evidence it helps people, and patients who’ve had such care are telling medical professionals that it’s “life changing, if not life saving”.
“The problem starts when these voices are excluded either directly – so either, they don’t exist for us, we don’t ask them what they think – or we create a kind of policy that says we discuss it, but, in practice, we do nothing about it,” the surgeon says.
“Let’s ask the people who receive it, and let’s believe them and go with what they want to achieve and how we can achieve that for them.
“The discussion derails completely when you have two cis, heteronormative people mostly from a rather financially affluent background. The discussion [is] between them on what is good and what is bad for other people. It doesn’t work like this.”
From his background as a breast surgeon, Ntanos has seen the power of patient advocates for women going through breast cancer or who are at risk of having breast cancer. He says advocate groups “have a voice”, “power over policies” and “power over waiting times”.
Yet, the same energy is not matched when it comes to giving trans people that voice in discussions on gender-affirming healthcare.
“Including a chapter like this [top surgery reference] in an international companion like that, we are in a sense giving a voice to the people who are going to request this type of surgery,” he says.
“It’s that. It’s reasonable.”
How did this story make you feel?

