Yes, lesbians can get STIs too: What to know about safe sex as a queer woman

Everything you need to know about safe sex as a queer woman ahead of Lesbian Visibility Week (Getty Images)
Ever been taught about the HIV risk for lesbians? Know what a dental dam is? If you’re a lesbian or a bisexual woman, chances are that most of your sex education has been cobbled together by hasty Google searches or asking your friends.
A common myth surrounding lesbian sex is that you can’t catch sexually transmitted infections (STIs). This couldn’t be more wrong. STIs can affect anyone of any gender or sexual orientation, and there are still risks for women who have sex with women (WSW).
This Lesbian Visibility Week, get clued-up on safer sex, and learn everything you need to know about STIs as a woman who has sex with women (WSW).

Can lesbians get sexually transmitted infections (STIs)?
Lesbians can indeed get STIs, with the most common within WSW communities being those that can be spread through intimate skin-to-skin contact, such as human papillomavirus (HPV) and herpes.
“From what we see in our clinic, and what we know from the data available in the UK, women who only have sex with other women do have significantly lower rates of most STIs compared [with] women who also, or only, sleep with men,” Marlena Segar, a sexual-health adviser at LGBTQ+-inclusive sexual health clinic 56 Dean Street, tells PinkNews.
“That isn’t to say, however, that women who have sex with women can’t or don’t get STIs from each other. Any contact where there is a transfer of sexual fluid with someone who has an STI, such as chlamydia, gonorrhoea or syphilis, has a possibility of transmitting that STI.
“Penetrative sex is the most common way STIs are transferred, so sharing insertive sex toys (toys used inside the vagina or anus) or masturbating and using the same hand to finger (or fist) your partner is more likely than oral or external fingering to transfer an STI.
“If you or your partner(s) are a trans woman, and you have penetrative sex, this can also transfer STIs fairly easily.”
Is HIV a risk for lesbians?
Experts have said that while contracting HIV is a very low risk for cisgender women who have sex with only other cisgender women, there are still issues of which queer women should be aware.
“Women who have sex with women are at a lower risk of getting HIV, there have only been two documented cases of women testing positive for HIV where the only possible cause could have been sex with another HIV-positive woman,” Segar said.
When cis women do test positive for HIV, it is more commonly attributed to another factor, such as injecting drugs, or having had sex with men, she added.
“What would make a transmission through sexual contact with another woman possible is the presence of blood and [the] sharing of sex toys.”
According to Aidsmap, trans women are more likely to have HIV, so for some trans lesbians, using condoms, taking the medicine pre-exposure prophylaxis (PrEP) and getting tested regularly, could be important steps to avoid infection.
It’s important to note that people who have HIV but who have been taking effective HIV treatment and have had an undetectable viral load for six months or more, cannot pass the virus on through sex. This is known as undetectable = untransmittable (U = U).
How can queer women have safer sex?
Lesbians and WSW can have safer sex by getting tested regularly, attending cervical screenings and, in some cases, using condoms or barrier protection during sex, according to the experts.
“The myth that women who only have sex with women can’t get STIs means many don’t have access to the sexual-health information and resources they need and are entitled to,” Segar said.
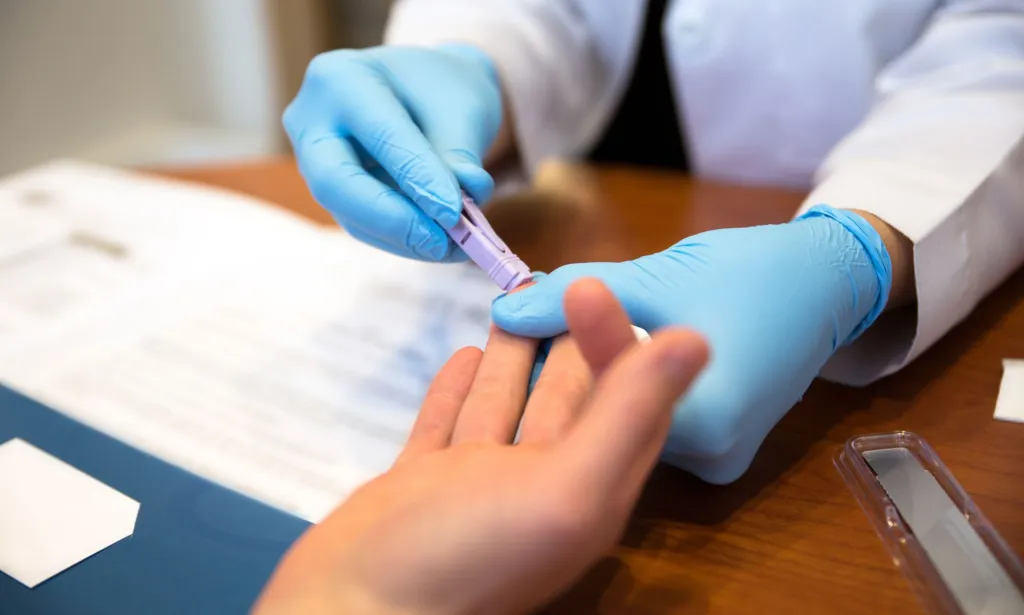
“It is possible to have an STI without experiencing initial symptoms. So, just as we would advise anyone else, regularly testing for STIs is an essential part of looking after your sexual health. We would recommend testing every three to six months, especially if you have more than one sexual partner during this time. Otherwise, we encourage a full sexual-health screen at least once a year.”
WSW can use “condoms when sharing sex toys, and dental dams during oral sex”, which can reduce the possibility of not just getting STIs, but also developing thrush or bacterial vaginosis, which aren’t technically STIs, but can occur after sex.
“Dental dams are thin latex sheets [essentially a flattened condom] that you hold against [your] vulva or bum during oral. If you don’t have access to dental dams, you can always cut a condom open and use it the same way,” she continued.
In some cases, HPV can be passed between cis women, and attending cervical screenings every three to five years is recommended, she went on to say. Adjustments can be made in the case of discomfort during smear tests, and you can book a double appointment or ask for a smaller speculum to be used.
“Since 2008, anyone assigned female at birth should have been offered an HPV vaccine at aged 12 to 13, at school. If you missed out, or if you moved to the UK after this, you can still get the vaccine free, up until the age of 25.”
Beat the stigma against STIs
The stigma surrounding STIs can be eased by communication, and talking to partners is a great way to have safer sex, Segar said.
“The stigma that still surrounds STIs often causes people to feel ashamed or scared to talk with a potential or current sexual partner about them. Remember that STIs are possibilities and not punishments for having sex.
“Despite the sex education you may have [had] at school that suggested otherwise, sex doesn’t revolve around STIs. A quick, honest conversation about them is more likely to ensure that you are protected.”
More widely, there can be a stigma for women and the LGBTQ+ community looking for medical help or advice, with eight per cent of queer people and 22 per cent of transgender men and women avoiding healthcare settings because of experiencing – or fearing – discrimination.
Finding an LGBTQ+-inclusive sexual-health clinic, or checking for STIs using a free at-home test kit can be a good way of getting a check-up for those uncomfortable using their local services.
Lesbian Visibility Week begins on Monday (22 April).
To learn more about HIV and Aids research, testing and treatment, visit amfar or the Terrence Higgins Trust.

