New mpox study examines NHS hospitals’ response to outbreak
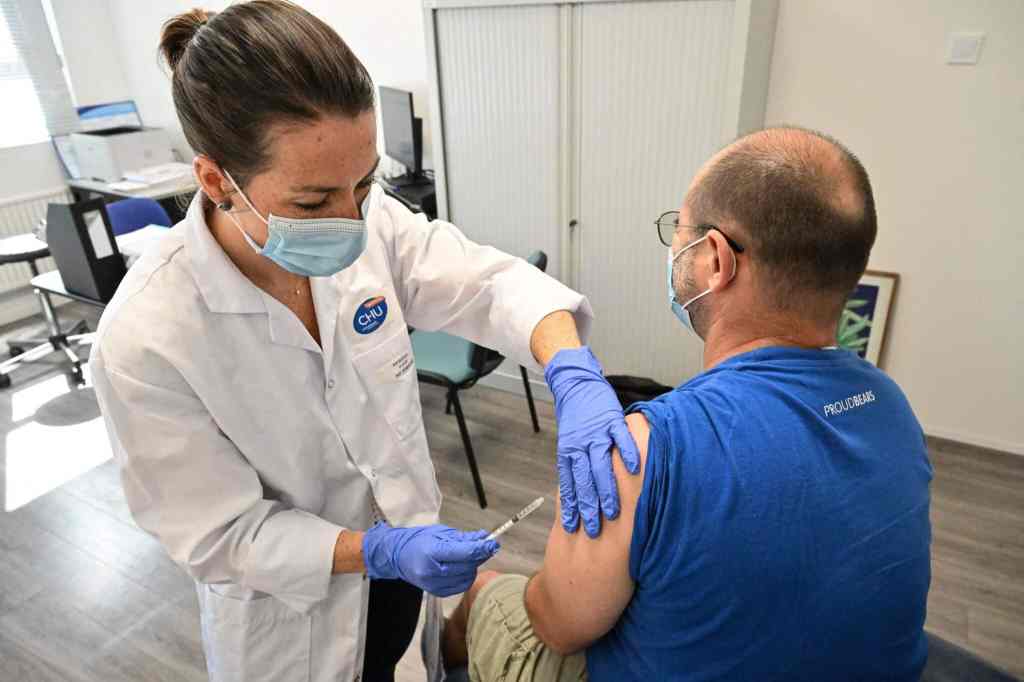
Experts are calling for ongoing mpox vaccinations across the UK as new cases are found in London. (PinkNews)
An infectious disease expert has praised access to healthcare in the UK as helping limit the severity of the mpox outbreak.
The 16 hospitals examined in the study “formed a virtual clinical network to manage the placement of patients, share information and experiences, and discuss case management including treatment options”.
In the report’s discussion, the authors said they believe this network “helped optimise inpatient care and knowledge-sharing for this emerging infectious disease in the UK” but urged for prospective studies and trials related to severe cases.
University College London infectious diseases clinical lecturer Dr Doug Fink, the report’s lead author, said access to “excellent medical care” in the UK for people living with HIV “may explain why we have seen very few people with untreated, advanced HIV infection and severe mpox”, formerly known as monkeypox.
He noted: “Other countries have reported severe disease and sadly some deaths, mostly in people living with HIV and who are immunosuppressed.”
Fink also said the study provided “the best estimate” of known severe mpox cases to be hospitalised, which was about five-to-six per cent for the period studied.
Published in the Lancet Infectious Diseases journal in late December, the report looked at the records and data of 156 people admitted to hospital with “complicated mpox” in 16 NHS hospitals across England and Northern Ireland between 6 May and 3 August, 2022.
More than half experienced “severe pain” and about a third of the patients were living with HIV, the report stated.
Most of those already living with HIV had a well-controlled infection and were not immunosuppressed.
One patient received their primary HIV diagnosis after being admitted to hospital.
Ten of the patients required surgery and there were two cases of encephalitis – serious inflammation of the brain.
The report stated there was a “need to share experiences of managing more severe disease” because mpox had been rare in countries outside Africa prior to 2022.
While there were “no clear differences in disease phenotype” between those living with HIV and HIV-negative people, the report said more research was needed to better understand risks and the natural history of mpox in people living with HIV.
A previous US study into mpox infections among people living with HIV described how the two “collided with tragic effects” for those not on effective treatment.
The report said the analysis was a “salutary reminder” that “mpox can cause a variety of complications in immunocompetent adults that often require multi-disciplinary inpatient management”.
The most recent data available from the UK Health Security Agency (UKHSA) shows there were 3,582 confirmed, and 148 highly probable, mpox cases in the UK between 6 May and 19 December 2022.
This UKHSA data overview was also the last time the figures were being published “due to low case numbers and availability of alternative reports”, the agency stated.
Numbers have been driven down by the adoption of a vaccine against mpox – though the UK government has been criticised for allowing stocks to temporarily run out, and for failing to launch a targeted information campaign.
How did this story make you feel?

